Introduction to Regulatory Revisions
According to the news (薬機法改正、審査の7論点を了承 制度部会、条件付き承認の見直しなど | 日刊薬業 – 医薬品産業の総合情報サイト) released by NIKKAN YAKUGYO on Oct/03/2024, Japan’s Ministry of Health, Labour and Welfare (MHLW) presented seven key proposals to revise the Pharmaceutical and Medical Device Act during a meeting of the Pharmaceutical Affairs and Food Sanitation Council. These proposals include improvements to the conditional approval system for prescription drugs, strategies to address drug loss in pediatric medicines, discussions on GMP inspections, and stable drug supply. The council will finalize the revision proposals by December, with legal amendments following.
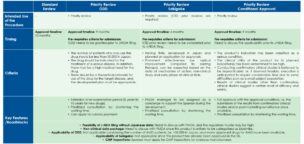
Changes to the Conditional Approval System
Unlike the US and European conditional approval systems, no regulation to revoke conditional approval after its commercialization has been set in the Japanese conditional approval system. This is why Japan has a higher hurdle to obtaining market approval, and there have been only a few cases in which the conditional approval system has been applied in Japan, unlike in the US and Europe. The government plans to introduce a revocation rule for the proposed revisions. In addition, the requirement to apply the system is revised from “cases shown clear effects in exploratory trials” to “cases reasonably predictable clinical usefulness “. This would allow us to expand the usage of the system and potentially speed up drug approvals.
Facilitating Expanded Clinical Trials
Japan also aims to simplify the procedures for expanded trials, ensuring better patient access to experimental treatments. This will streamline clinical trial processes, supporting local and international drug development efforts.
Extended Re-Examination Periods for Pediatric Medicines
To deal with the drug loss issue in pediatric medicines, MHLW proposes that pharmaceutical companies be obligated to establish pediatric drug development plans when applying for drug approvals. The re-examination period for such pediatric drugs would be extended by two years—normal drugs from eight to ten years and orphan drugs from ten to twelve years—offering incentives for companies to invest in pediatric drug development.
Recognition of Real-World Data in Drug Applications
MHLW is also working to enhance the use of real-world data (RWD) in drug approval applications. The ministry intends to amend the law to clarify that RWD can be used in regulatory submissions, raising awareness of RWD’s potential to support faster approvals.
Addressing Drug Supply Shortages
To mitigate the impact of drug shortages, Japan plans to introduce new regulations allowing the fast-tracked approval and distribution of alternative overseas products during critical shortages. Special measures will also allow the use of foreign-language packaging for a limited time. These steps aim to prevent supply disruptions in the healthcare system.
Streamlining Manufacturing Change Approvals
Revisions are proposed to shorten the review period for moderate-risk changes in drug manufacturing processes from six months to 40 days. Additionally, the cap on monthly applications for process changes would be lifted, facilitating faster implementation of manufacturing improvements.
Advancing Harmonization with Foreign Pharmacopeias
Japan is working to harmonize its pharmacopeial standards with international ones, addressing bottlenecks faced by companies importing foreign-made drugs. This will simplify the approval and supply process for imported pharmaceuticals, ensuring timely patient access to medicines.
Enhanced Access to Regenerative Medicine
In a humanitarian move, Japan will allow pharmaceutical companies to provide regenerative medicine products that fall outside the usual standards if they meet specific criteria, improving patient access to advanced treatments. The government’s safety relief program will also cover such cases.
Conclusion
Japan’s proposed Pharmaceutical and Medical Device Act revisions aim to modernize the regulatory environment, enhance drug accessibility, and foster innovation. These changes will benefit domestic and global pharmaceutical companies by creating a more efficient drug development and approval pathway. The next meeting to discuss these proposals is scheduled for October 31st.